True story TRIGGER WARNING
There are many wonderful, supportive obstetricians and I adore the ones I am blessed to work with. But sometimes I do hospital shifts, or help advocate for people in the hospital and have personally seen things that make me cringe.
I was to labor at home with a friend’s daughter expecting her first baby as long as possible. I brought her in fully dilated with no urge to push yet. At midnight, the only door open was through the emergency room. We were told to go the waiting room. Wearing eye pads and head phones in a public area, mama slow danced with me over 2 hours. Then she suddenly roared baby’s coming. I asked the person sitting at the desk several times to please get her up to the maternity unit as soon as possible. The staff person kept saying she needs to be seen first in triage, so need to go back to waiting room.
I said “she is pushing and saying her baby is coming as you can see. There is no more time to wait. We've been waiting over two hours.” Lady said it's hospital policy - she has to be seen first by a doctor in triage to determine if she needs to be admitted.” I said “I don't care about policies that make no sense. You can see this mama is having a baby, now. I'm a midwife, I know how to catch a baby here in the waiting room but I don't have privileges in this hospital and here is not the best place for her to give birth.” She rolled her eyes, told me there is nothing she can do, and said “next” to the person behind me. Mama is continuing to roar, saying “baby’s coming out!!!”
I rushed to a security guard standing in front of a bunch of wheel chairs. I told him I needed one stat to take this imminently birthing lady up to labor and delivery. He was at least nicer about it but said “he's sorry that he's not authorized to give one to me.” And what do you think I did? I stole one right in front of him, he looked stunned but did nothing, I took mama up to the maternity unit breaking all kinds of hospital rules.
But really? What would have happened if that was just herself and partner, no advocate? They would have had an ER waiting room birth, in an atmosphere of neglect and then chaos.
As soon as we got into the room, the staff was undressing her and put her into a hospital gown. Some battles aren’t worth the fight, and she did not care at this point, what she was wearing or not wearing. As I am supporting her in the hospital room, she assumed hands and knees position on the bed and continued to push. I could see baby’s head with each push. Multiple people came in, to draw blood, get her admitted by asking all kinds of irrelevant questions - like how much weight she gained in pregnancy as she was pushing; several nurses were trying to get her to lay down to get a continuous fetal monitor strip and start IV. I said she declines both, and intermittent listening to baby’s heart rate was her preference and is sufficient. Mama anyway kept insisting she needed to be on her hands and knees and resumed that position. I then see baby’s head crowning (emerging from the vaginal opening), and prepare for birth.
I suddenly heard mama shrieking, begging for me to help and make the doctor get out of her butt hole. I could not believe what I then witnessed. An obstetrician was doing a rectal exam, obviously without her consent, she was resisting, and he started yelling at her. Mama continued to scream to get him out of her. He continued to yell at her saying he needs to check if she is fully dilated. For those of you who don’t know, if baby is crowning, there is no more cervix, so of course mama is fully dilated. And to check the cervix you need to do a vaginal exam. It’s not accessible through the rectum. Nurses rolled their eyes as he was in the wrong place and his exam was not needed anyway. Help! Don’t let him touch me she pleaded.
I said I was a midwife, her advocate, her midwife is on the way (just changing) to take over as it’s her case, I am not sure why he was in there anyway, what he was doing was abusive, and he would be reported. He left in a huff.
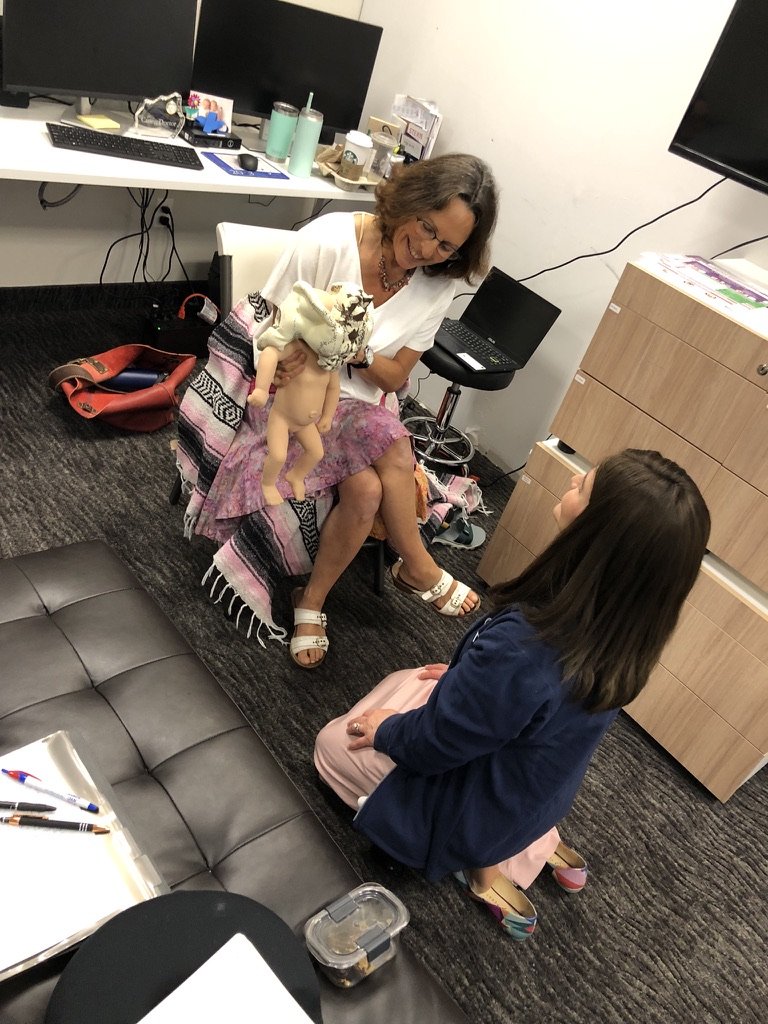
I looked mama in the eyes, said I was sorry for what was done but she is safe now, it’s good to be on her hands and knees. I reassured her that Baby’s heart rate was fine by Doppler, and reminded her to breathe. We breathed together as her baby gently slipped into midwife’s hands. She cried, and was so thankful…but part of the tears was how she was treated initially. I held her in her pain. Just practicing midwifery. THIS ABUSE HAS TO STOP. He was reported to no effect!
Mama and baby were wonderfully healthy, she was amazingly able to tune it all out with her eye pads and head phones, and actually loved her birth but joked her situation at the hospital was like a sit com. But…”Next time just staying at home” she said. She did not want to pursue any other action against the doctor.
Share this! We must improve maternity care. We must know what is going on with our bodies and what to expect, have an advocate or doula especially if its your first and you are planning a hospital birth, speak up and make the choices best for us.
To learn more what you can do whether you are planning to birth in the hospital, at a birthing center or home, to have the birth YOU want & will treasure forever, check out my signature comprehensive Love Your Birth online prep Guide to Pregnancy, Birth & Postpartum prep course and in adjunct my Natural Birth Secrets book 2nd edition, for deep dive into the hot topics and research.
Story told with permission.