Embracing the Journey of Discomfort✨
Feeling aches in your pelvis, legs, or back during pregnancy can be humbling—but it’s also a powerful opportunity for growth. These sensations invite you to lean into mindful breathing, self-compassion, and deeper connection with your changing body.
Who Can Help (Think Natural Therapists!)
Before diving into self-care, consider reaching out to trusted holistic practitioners:
Chiropractor or osteopath — reset pelvic alignment
Massage therapist (deep tissue, Thai, Rolfing) — ease muscle tension
Homeopath — custom herbal or flower remedies
Acupuncturist — targeted needle therapy
Therapeutic yoga instructor — build strength and ease tightness
🌿 Round Ligament & Groin Pain
Sharp pangs in your groin—especially when walking or stretching? Here’s how to soothe and prevent them:
Rest, then rock: Lie on your back, knees bent, or get on hands & knees and gently rock your pelvis
Soak & soothe: Warm Epsom salt bath with lavender or herbal blends, followed by Tiger Balm and a hot/cold pack
Support: Use a pregnancy pillow and maternity belt, like the Bellefit supportwear
Strengthen: Practice pelvic-floor exercises—bridge pose with mula bandha (root lock) on a yoga block builds core support and tone
🔙 Upper & Lower Back Care
Upper back: Breast changes can strain your shoulders. Wear a supportive bra and stretch regularly with shoulder rolls.
Lower back: Weight shift, ligament loosening, and posture changes contribute to discomfort. Try:
Prenatal belts (e.g., Baby Hugger)
Gentle yoga postures (cat/cow, sphinx, bridge) - I teach this in my online yoga classes.
Mindful lifting and posture (tuck in your pelvis, avoid high heels)
🔥 Sciatica Relief
Sciatic pain (sharp, radiating from your back down your leg)? Try:
Exercises: Hamstring stretches, spinal twists, standing hip openers
Stay active: Daily walking, swimming, low-impact movement
Anti-inflammatory diet: Whole foods, turmeric-rich meals, hydration (64 oz+)
Targeted yoga: Tailored stretches to decompress irritated nerves
Smart Movement & Body Mechanics
Rest when needed: Lighten your load—delegate more, schedule breaks
Posture check: Stand and walk with lifted abdomen, tucked pelvis, relaxed shoulders
Sneakers, not heels: Flat, supportive footwear—barefoot at home feels amazing
Lift right: Bend at knees, use core support, avoid twisting
Safety first: Take extra care on slippery surfaces, add non-slip mats
💤 Supportive Sleep & Rest
Comfort while resting is essential:
Bedding: Firm mattress or board; pregnancy pillow for side sleeping
Environment: Cool (mid‑60s°F), dark, quiet—blackout curtains, eye masks, white-noise machines
Rituals: Early bedtime, gentle stretching, warm herbal teas, and peaceful wind-down routines
🧘 Healing Through Breath & Relaxation
Pain often arises from tension. Here’s how to ease it:
Deep abdominal breathing – In for 4, out for 4
Box breathing – In 3, hold 6, out 6, hold 3
Relaxation scan – Tense and release muscles from head to toe
Ujjayi breath – Gentle ocean-sound breath awareness
These techniques calm your nervous system and teach your body to relax into sensations, not fight them—a vital skill for labor and beyond.
🛠️ At-Home Remedies for Back Pain
Massage oil blend: Arnica + St. John’s wort + cramp bark + essential oils (ginger, lavender, or rosemary)
Heat or ice: Alternate cold packs (first 24–48 hrs) with moist heat (showers, Epsom baths)
Healing yoga pose: Legs Up The Wall—rest on your back with legs up against a wall or bolster for 10–20 minutes.
Herbal support: Tinctures like cramp bark, skullcap, St. John’s wort, plus turmeric for inflammation. Reputable brands of the supplements and remedies I recommend include any of those in my online holistic apothecary.
TENS unit: Safe, drug-free pain relief option (often works well during labor too)
🌀 Supporting SPD (Symphysis Pubis Dysfunction)
SPD can feel intense, but these gentle supports help:
Chiropractic care + support belts (Bellefit, Baby Hugger)
Pelvic floor activation before movement
Gentle repositioning: Keep legs close and move slowly when turning or rolling
Seek help: If walking forward hurts, backward feels better—consider physical therapy or crutchesTo release stress and trauma energy often responsible for chronic issues, do conscious connected Clarity breathwork and experience miraculous healing and transformation. Also check out Brandon Bays’ book The Journey, and her website. These are all extremely effective mind-body cutting edge methods that have also lead to transformational healing for thousands of people around the world.
🧠 When Pain Persists or Feels ‘Off’
While many aches are pregnancy-related, check in with your provider if you experience:
Severe, persistent pain
Fever, bleeding, bladder/bowel changes
Leg swelling/redness (possible blood clot)
New or unusual symptoms
Chronic pain solutions may involve mindful emotional work—think The Mindbody Prescription or Clarity Breathwork to release underlying stress and trauma.
📅 Your Personalized Well-Being Plan
Gentle movement – Yoga, walking, swimming
Core & pelvic care – Strengthen with awareness
Supportive gear – Maternity belts, pillows, sneakers
Healing tools – Massage blends, heat/ice, TENS
Breathing & mindfulness – Your daily reset toolkit
Rest intentionally – Sleep earlier, nap strategically
Connect & empower – Video guidance or local sessions
📞 Let’s Connect
Need personalized guidance? Book a video consultation with me—we’ll chart a gentle, effective plan tailored to you and your baby.
Pregnancy is a time of profound transformation. Your body is working hard—reward it with kindness, awareness, and nurturing care. 💛
You’ve got this, mama..
Photo by Megan Hancock Photography
Let Me Help You Create The Happiest Birth Experience Of Your Life...
Whether you're a first time or experienced momma,
Or a midwife, doula, or birth professional guiding mommas..
Regardless if you are planning a birth at home, a hospital, a birth center or need a cesarean section, or if you are taking another childbirth education class…
You Really Can Create The Delivery Of Your Dreams.
And have a blissful birth wherever you are.
More Precious Than A Wedding...A Birth Should Be A Celebration!
Let me show you how to…
Understand the sensations of your body and connect your intuition with how your body is communicating and leading you towards what to do during labor
Tap into your inner calm to deeply relax yourself,letting go of busy, stressful and fearful thoughts on demand for the health of baby
Speak your truth from your heart in a way that deepens your relationships, sets clear boundaries, and has people listen to you and support you before, during and after pregnancy
Trust yourself, connect with your body wisdom andcommunicate with baby in belly
Connect with natural time and sync your body and mind up with your unique biological clock for ease from pregnancy to postpartum
Reprogram negative patterns, stories, and beliefs that undermine your confidence, strength and self trust so you can rock your birth
Physicians and midwives around the world recommend my teachings to their pregnant clients and many Doulas across the country learn the secrets of blissful birthing from me to supplement their Doula Training & Certification process!
To learn more, visit: LOVE YOUR BIRTH Online Childbirth Course!
It is based on my years of experience, as a midwife and yoga teacher, helping thousands of women tap into their calm and live and birth from a place of grounded relaxation and joy.
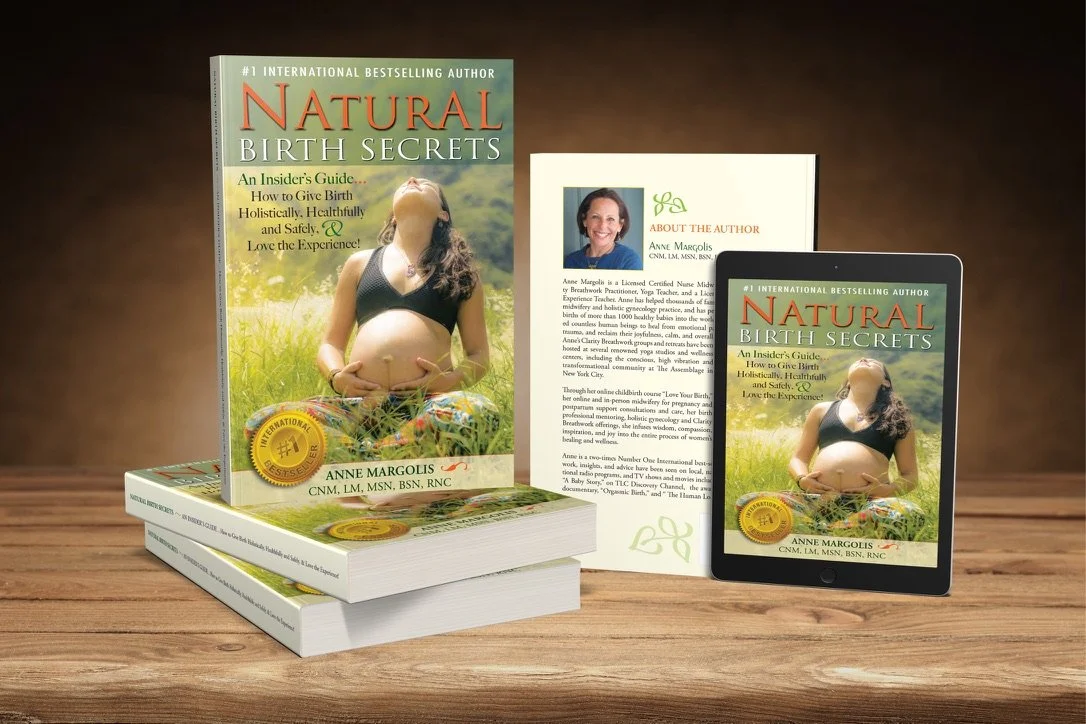
Check out my Natural Birth Secrets book 2nd edition as your reference for more in depth information on holistic modalities for all common discomforts and ailments on your entire journey to having a baby - from preconception, through pregnancy and postpartum, as well as breastfeeding and newborn care.