I come on here in a very honest and vulnerable place, but I feel it is important to share my thoughts with you, and where I stand on this matter!
I totally understand where many of you are coming from in wanting to stay out of standard hospitals that are failing healthy expecting families, and many do not feel they have other local options and want alternatives. Totally! I get the limited options for VBAC, twins, breech birth and even going past due date. I get the financial and insurance limits. I get that people are feeling some midwives act more like doctors or practice too medically. I get wanting privacy and to feel completely safe without any interference, and the potential negative effect of anyone’s behavior, even well-meaning, on your emotions, stress labor and ultimately labor during such a sensitive and sacred time as giving birth.
Those wanting a homebirth or birth center birth are not getting the support they need either as there are not enough trained homebirth midwives or birth centers to go around. Even midwives who want to practice home or birthing center birth are bound by legal restrictions or their hands are tied by collaborative back up unsupportive physicians and hospitals. Many licensed legal providers are also restricted by state regulations, insurance policies, local standard of care, and even each of their own comfort level and sense of safety, fears related to previous bad outcomes impacting their current care. I get it. My heart goes out to all of you. I will continue to do my best to help.
But I can not keep quiet about planned unassisted freebirth at home. I implore you to find a homebirth midwife, if you want a homebirth. I must uphold safety of mom AND of baby, who does not have a say in this discussion. The research supports the safety of homebirth with homebirth midwives, NOT without them. Those whose planned unassisted freebirth went well are blessed. I fully support unassisted birth in all settings...with midwife there in the background at least as a lifeguard just in case. As a homebirth midwife for nearly three decades, who has also worked in birth centers and supportive hospitals, I have seen enough situations in which healthy mom and/or baby had an unpredictable complication or emergency and would have been seriously damaged or died had I or another trained attendant not been there to literally and immediately save their lives. Period. Time was of the essence. Your midwife is ideally, at least the lifeguard for you and your baby. For the rare and uncommon. Many mamas want the full midwifery supportive care experience and all of the other benefits that come with having a wonderful authentic midwife. Part of that care is having a close relationship where you feel heard, respected, safe and secure, where there is full trust in a healthy women’s ability to grow, birth and breastfeed her baby until proven otherwise. Yes, most births go well, and all is beautiful & groovy...until it is not, and then it is so not groovy. That is when you REALLY need an excellent midwife. I have helped families with train wrecks of tragic disasters transferring to a hospital too late from a freebirth when I do shifts in the hospital. I also had to help countless women who reach out to me for guidance and help processing and healing the trauma, the shame and guilt of an unassisted birth gone bad. This is not the typical fear mongering you get by the medical profession, fearing you into unneeded risky interventions when all is well. It is a legitimate real danger, and it is not a subject I can simply sugar coat. It is you and your baby’s life at stake. The freebirth movement is doing you a disservice by telling you otherwise, that there are risks in everything, that you can train to resolve any birth emergency, even shoulder dystocia and postpartum hemorrhage - which is so not true. And I have devoted my entire career to empower women. I am also grateful for awesome midwifery and even medical/surgical care when needed and lifesaving. These are not contradictory.
Go deep. Meditate on what is best for you and your baby, how you would feel if that happened to you. Or if you went to the hospital as planned & some disaster happened. Make sure you could live with your decision no matter what the outcome. Then you will labor best where you are most comfortable, knowing there are never any guarantees in this field. And do consider the options of traveling more of a distance to get a midwife, like people traveled to Ina May Gaskin’s center at the Farm in Tennessee to get the birth they wanted. Or hire a traveling midwife. You may also be able to find the most supportive midwife or obstetrician and birthing center or hospital and exert your legal right to have a completely beautiful undisturbed physiologic birth through postpartum without any intervention unless absolutely medically necessary and life saving.
I have helped many mamas achieve just that. It takes research, preparation and advocacy, having lots of conversations with your provider and setting in pregnancy but is more doable than you might think. A mama took my Love Your Birth online prep course and respectfully convinced a very medical obstetrician with high rates of induction and cesarean - her only local option, who has not even seen natural birth - to be there outside her room, just in case, until the actual birth. She surrounded herself with support she needed while in labor. Not only did she have a transformative empowered birth experience she dreamed of and planned for, but her doctor was completely humbled, transformed and brought to tears as well….just think of the ripple effect that will have on his future practice for other mamas! Also there are many authentic wonderful midwives out there who do support undisturbed beautiful birth and have holistic approaches - there are different type of midwives….you might just need to dig deeper and do more research. This is one of the most important days of your life. Choose wisely.
Let me help you have a deeply positive, empowering and joyful journey through pregnancy, birth and being a momma in postpartum with my LOVE YOUR BIRTH online course.
I’ve taken everything I’ve learned, trained and supported women with locally for nearly 30 years in my private practice and I’ve poured all of my love, passion, knowledge and experience into creating something truly special for you....My Love Your Birth online comprehensive prep course. Check it out now!
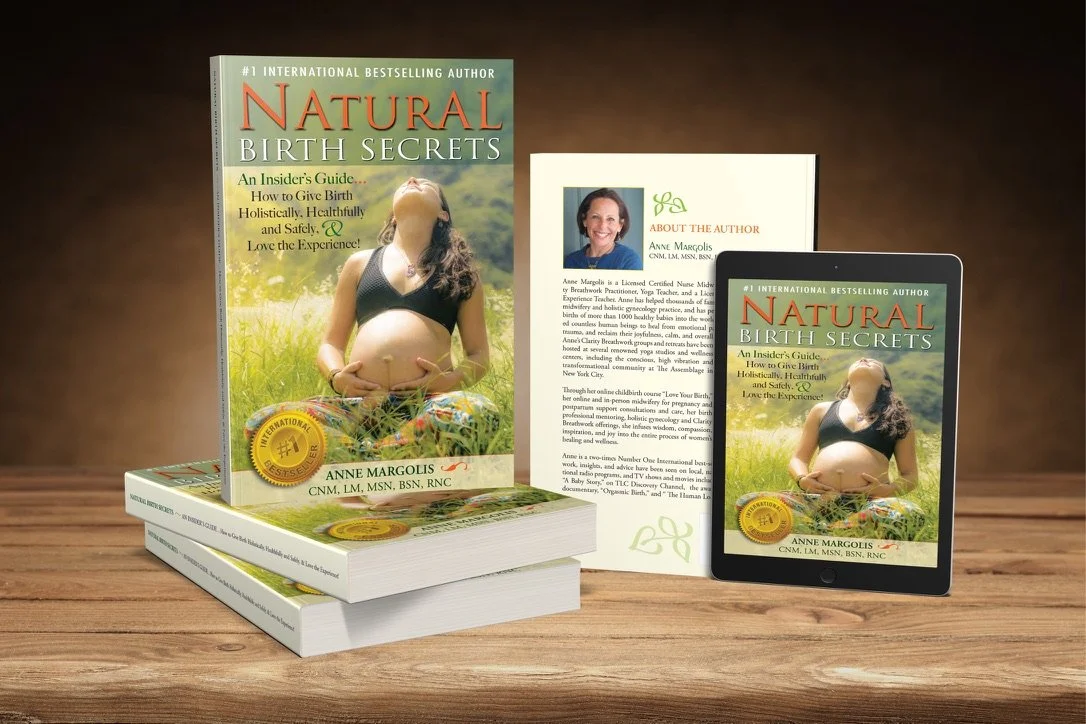
Educate and inspire yourself, ready your body, ready your mind, ready your heart with my list of TOP BOOKS of every category you can imagine listed - with links on where to get them as books, listen on audio, or read them on kindle. The better prepared we are for a situation, the better the outcome will be. I feel passionate about empowering and educating women to get the most out of their womanhood, pregnancy, birth, postpartum, breastfeeding, mama, yoga and life journeys!