Let’s be real—pregnancy can make sleep feel like a distant dream. Between aches, baby kicks, hormonal shifts, and an overactive mind, insomnia becomes an unwelcome visitor for many expecting mothers. As a holistic nurse midwife, I often hear, “I’m tired but I just can’t sleep!”
The good news? You’re not alone—and there are safe, natural ways to support restful sleep during pregnancy. Let’s dive into gentle strategies to help your body relax, your mind slow down, and your whole being settle into deep, restorative rest.
💭 First, Don’t Panic If You're Awake at 3 AM
If you’re managing to function during the day, your body might be getting enough rest even if your sleep feels broken. But if you're feeling exhausted, burnt out, anxious, or moody, it may be time to make sleep a higher priority—right up there with eating well and moving your body.
Pro Tip: If insomnia was a struggle before pregnancy, check in with a holistic or integrative provider to rule out deeper causes like thyroid imbalance, anxiety, or chronic stress.
🌿 Natural Insomnia Prevention: Start with the Basics
Here’s what to avoid 4–5 hours before bed to help you wind down easier:
🚫 Caffeine (coffee, tea, chocolate, soda)
🚫 Heavy meals or processed foods
🚫 Excess fluids (to avoid 3 am bathroom breaks)
🚫 Emotional or intense conversations
🚫 Scrolling social media or news
🚫 Blue light (from screens)
🚫 Vigorous workouts
Instead, opt for calming routines, gentle stretching, and a light snack that balances blood sugar—think gluten-free oatmeal with nut milk, or apple with nut butter.
🛏️ Honor Your Sleep Rhythms
Your body has a natural clock, so give it the rhythm it craves:
🕙 Aim to go to bed around the same time each night (ideally before 11pm)
🌞 Get sunlight during the day—especially morning light
🌚 Keep evenings dim—use amber lights, candles, or salt lamps
❄️ Sleep in a cool room (mid-60s°F is ideal)
📵 Keep phones and computers out of your bedroom (seriously!)
Need to break up with your phone at bedtime? Check out “How to Break Up With Your Phone” by Catherine Price—your nervous system will thank you.
🧘♀️ Make Evenings Sacred: Your Wind-Down Routine
Design a nighttime ritual that feels like a warm hug:
🛁 Soak in an Epsom salt bath with lavender or chamomile oil
📖 Read something soothing—not thrilling
🧘♀️ Try 5–15 minutes of Yin or restorative yoga
💨 Do calming breathwork (more on that below)
🎧 Listen to relaxing music or use sleep meditation apps. 🌬️ Breathe Your Way to Better Sleep
When stress is high and your mind is racing, your breath is your superpower. Try these simple exercises:
🌸 Deep Belly Breathing
Inhale for 4 counts
Exhale for 4 counts
Repeat 8 times
Want more calm? Extend your exhale—inhale for 4, exhale for 6.
🔲 Box Breathing
Inhale 3
Hold 6
Exhale 6
Hold 3
Repeat for 5–10 minutes
💨 Forced Exhalation
Breathe out completely
Let breath naturally come in
Repeat for a few minutes
These practices calm your nervous system and help your body switch from “fight or flight” to “rest and digest.”
🪷 Stress Reduction = Sleep Support
Stress and pregnancy go hand in hand—but you don’t have to stay stuck in high gear. Here's how to find your inner calm:
✨ Set boundaries and say “no” when needed
✨ Ask for help (yes, really!)
✨ Take “healing intervals”—short breaks to do nothing
✨ Practice mindfulness, meditation, or yoga - (especially Yin, prenatal, gentle and restorative)
✨ Surround yourself with people and environments that feel safe and soothing
☕ Bedtime Teas & Natural Remedies
Try these gentle, nourishing herbal teas to sip in the evening - many are available in my online holistic apothecary.:
Evening Sleepy Tea Blend
Chamomile
Lemon Balm
Lavender
Steep 1 tsp of each herb in hot water, cover for 15–20 minutes, strain and enjoy. Sweeten with a little honey or lemon if you like.
Magnesium & Calcium
Take 500–1000 mg magnesium (Natural Calm is a great option)
Pair with 500–1000 mg calcium if needed
Herbal Support (after first trimester):
Passionflower – for anxiety-related insomnia
Chamomile tincture – gentle and safe
Skullcap, Lemon Balm, or Motherwort – calming nervines
CBD (from pure hemp oil) – gentle calming (talk to your provider first)
Need more targeted support? Look into flower essences like White Chestnut for racing thoughts, or consult a homeopath or naturopath for customized guidance.
🛌 Sleep Hygiene 101
Let’s set the stage for sleep success:
Keep your bedroom cool, dark, quiet, and device-free
Try blackout curtains, an eye mask, or white noise
Use a supportive pregnancy pillow and comfy bedding
Avoid work, bills, or screens in bed
Get a real alarm clock (not your phone!)
🌿 Natural Supplements (Use With Care)
Here are some options to explore—always check with your provider before adding supplements and herbs during pregnancy:
Fresh milky oat tops tincture – supports the nervous system over time
Collagen powder (grass-fed gelatin) – mix into evening oatmeal
Valerian root, St. John’s Wort, Lemon Balm – occasional use only
Melatonin – best for travel or shift work (not everyday use)
💤 When You Just. Can’t. Sleep.
It happens. When you’re lying awake, try:
✔️ Reverse psychology: Tell yourself to stay awake—ironically, it can help you fall asleep.
✔️ Get up and do something low-key: fold laundry, read, or listen to soft music.
✔️ Write down worries and make a plan for the morning.
✔️ Don’t fight it—rest is still valuable, even if you’re not fully asleep.
Final Thoughts
Pregnancy is a time of great transformation, and your sleep patterns will shift. That doesn’t mean you’re powerless! With simple, consistent habits, a few calming herbs, and a whole lot of self-kindness, you can get the rest your body needs.
Let sleep be your sacred time. You’re not just nourishing your growing baby—you’re replenishing yourself.
If you need more personal guidance, schedule an online video call or a breathwork session with me.
💛 Wishing you deep rest, sweet dreams, and a peaceful journey into motherhood.
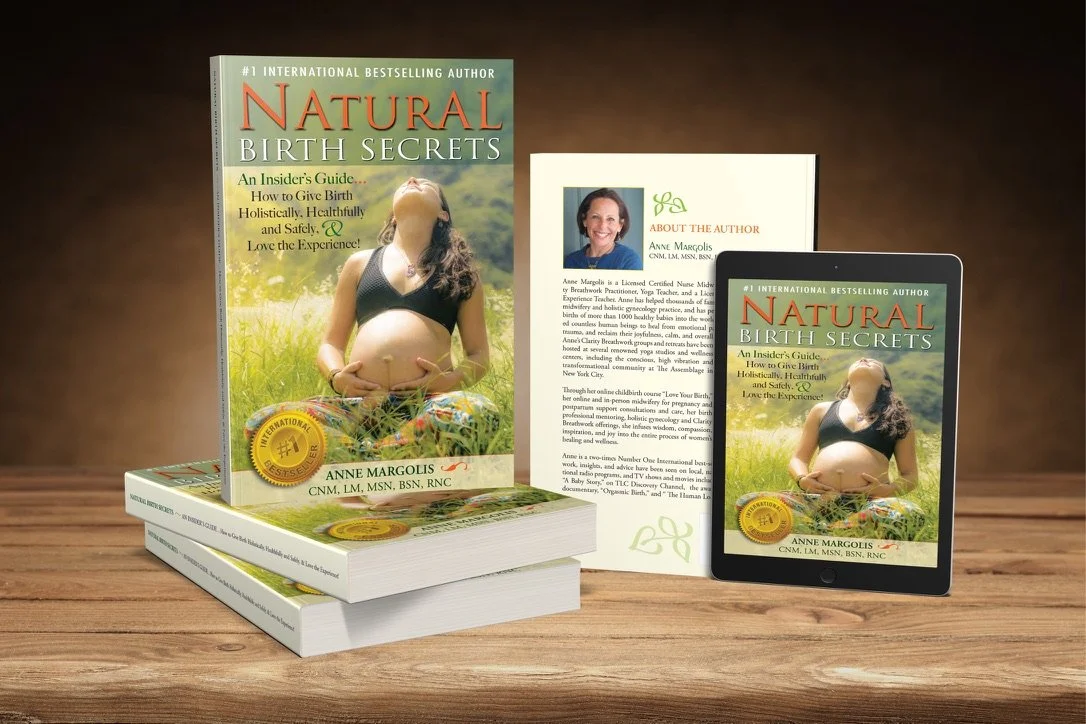
Check out my Natural Birth Secrets book 2nd edition as your reference for more information on holistic modalities for all common discomforts and ailments on your entire journey to having a baby - from preconception, through pregnancy and postpartum, as well as breastfeeding and newborn care.
Let Me Help You Create The Happiest Birth Experience Of Your Life...
Whether you're a first time or experienced momma,
Or a midwife, doula, or birth professional guiding mommas..
Regardless if you are planning a birth at home, a hospital, a birth center or need a cesarean section, or if you are taking another childbirth education class…
You Really Can Create The Delivery Of Your Dreams.
And have a blissful birth wherever you are.
More Precious Than A Wedding...A Birth Should Be A Celebration!
Let me show you how to…
Understand the sensations of your body and connect your intuition with how your body is communicating and leading you towards what to do during labor
Tap into your inner calm to deeply relax yourself,letting go of busy, stressful and fearful thoughts on demand for the health of baby
Speak your truth from your heart in a way that deepens your relationships, sets clear boundaries, and has people listen to you and support you before, during and after pregnancy
Trust yourself, connect with your body wisdom andcommunicate with baby in belly
Connect with natural time and sync your body and mind up with your unique biological clock for ease from pregnancy to postpartum
Reprogram negative patterns, stories, and beliefs that undermine your confidence, strength and self trust so you can rock your birth
Physicians and midwives around the world recommend my teachings to their pregnant clients and many Doulas across the country learn the secrets of blissful birthing from me to supplement their Doula Training & Certification process!
To learn more, visit: LOVE YOUR BIRTH Online Childbirth Course!
It is based on my years of experience, as a midwife and yoga teacher, helping thousands of women tap into their calm and live and birth from a place of grounded relaxation and joy.