Just a taste of a much larger discussion. History for most of history was mostly ‘his story’. Through the majorly of it, women were mostly illiterate as they were not allowed to be educated like men. But until relatively recently, men would not provide care for women and their gynecological and childbearing needs even when they became physicians - as their reputations would be tarnished if they associated with women’s genitalia and their business. It was the domain of women. Women supported women.
Midwifery is mentioned as far back as biblical times, and recorded in Egypt as early as 1900 BCE. Birth was a normal part of family life, men were kept out, and certain women in each community took on the role as midwife, by following and learning from the elder midwives. They used natural remedies. Some did secretly train under physicians. In the medieval times, there are some conflicting historical accounts whether or not they were falsely accused of witchcraft and were persecuted- especially when some unsuccessful outcomes became apparent, their lack of formal training, and use of natural remedies - all a catch 22, as they were not allowed to do formal training or to practice medicine, had no access to medicines, so they used natural remedies, and were thought to go against the church, medical hierarchy and legislature which were often intertwined.
Today, thankfully there have been many beneficial changes like standardized formal education for women in the practice of midwifery, which includes sexual and reproductive health as well as equal rights of women in most developed countries. We do have a way to go in the United states and other countries, as barriers and obstacles to midwifery practice still exist. Midwifery is respected by the medical profession and encouraged for low risk population by leading health organizations. It’s now organized into a profession and supported by legislation as well as biblical religions. Hard to do the real history of midwifery justice in a blog, but at least I can reassure you I am a good witch.
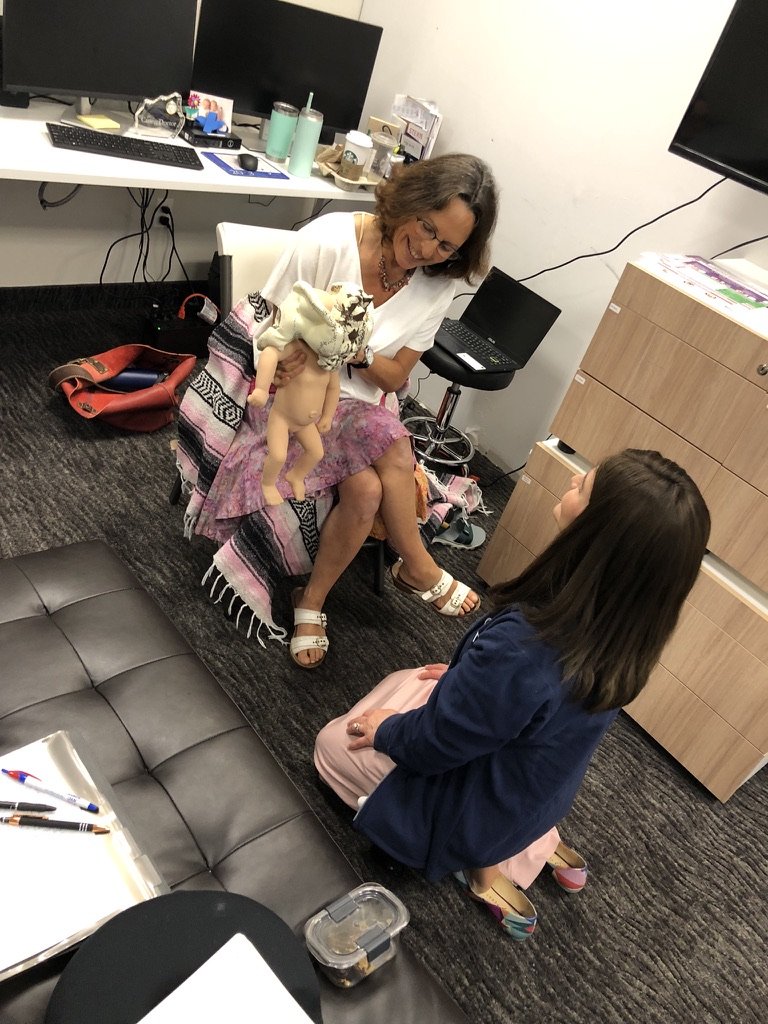
I’ve taken everything I’ve learned, trained, and supported women locally for over 28 years in my private practice and I’ve poured all of my love, passion, knowledge, and experience into creating something truly special for you… my new and updated Love Your Birth Pregnancy, Birth & Postpartum Guides. Same Beloved Content Plus Over 20 Added Bonus Videos! Buy Here Now!
They can be used via the mobile App or on your desktop! It’s the most up to date combination of Love Your Birth and Walk With Anne for Mamas online courses at a cheaper price! And they have an option for direct access to me for your questions and concerns!!
Whether you’re an experienced or new parent, there are hours of videos, workbooks, and PDFs to answer all of your questions. Everything is searchable, so you can just type or talk and it’ll bring you right to the exact moment in the video where I answer your question. It’ll blow your mind! If English is not your strongest language, you can even change the captions or even the audio to the language you prefer. You can the Love Your Birth Prenatal, Birth & Postpartum Guides -ALL of the guides for a limited-time offer of 50% off -> RIGHT HERE!
The key to a positive birth is feeling confident, strong, relaxed, and empowered during the entire process, regardless of the twists and turns it may take. I give my full heart and all I know in everything I do to support Mommas.