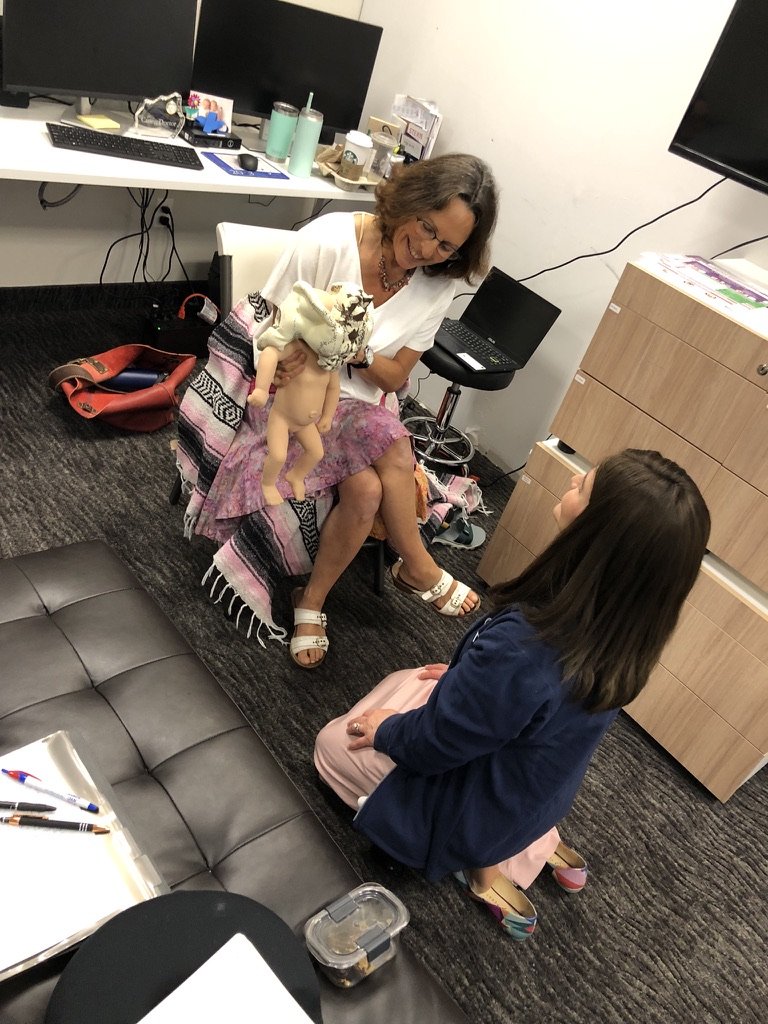
So grateful to Dr. David Hayes OBGYN @breechwithoutborders for their amazing continuing education workshop to thoroughly review the data and teach skills of attending vaginal physiologic breech birth globally. Some key take aways are: 📣Modern US clinicians and hospitals, and other countries that follow US, where only cesarean is taught and practiced for breech - please get back your skills and follow ongoing current impressive research and guidelines of other western countries where upright vaginal breech birth is being heavily studied and practiced as the norm, as it has been among community out-of -hospital midwives around the world through history.
More & more mamas don’t want c-section and all the risks associated with major abdominal surgery for them, their babies, and future fertility as the only option, and are seeking safe alternatives. Breech presentation occurs at term ~ 4% of the time ,vast majority are called frank with hips flexed, legs extended upward. Sometimes they can be turned head down to vertex presentation, sometimes they can’t and are breech for a reason. It’s very rare for a term baby to stand in the uterus, presenting one or two feet first - which is usually NOT footling (a common misdiagnosis) but complete or incomplete breech - hips flexed, buttocks in pelvis like a frank breech but one or two legs flexed, with one or two feet dropped down. These presentations in healthy pregnancy are fine candidates for term vaginal breech birth. It’s crucial for providers to know when to keep hands off, support mamas own movement and pushing efforts, upright positioning, how to resolve uncommon stuck arms, shoulders and head behind the pelvic bones, monitor baby’s condition, expedite birth and effectively resuscitate baby if needed.
Significantly less invasive maneuvers are required in physiological breech birth in upright positions with improved outcomes for mamas and babies. For mamas, breech birth is often claimed to be easier than birthing babies in head down position, with less injury to pelvic floor muscles and reduced tearing. Those I’ve attended all went well. The trouble and poor reputation associated with vaginal breech birth are mostly caused by unskilled providers, keeping mama on her back, impatience & pulling - which skewed the data of the older term breech trial they still quote. If you have a persistent breech baby know you have options. Get true informed consent!
If you’ve been told that your baby is breech at your mid pregnancy anatomy scan, know that baby is still swimming and it is likely they will be head down by term. If baby is breech later in the third trimester, don’t freak out. There are many ways to gently and lovingly ease your baby into vertex. Since there is slightly greater risk to breech babies born vaginally and by cesarean, and many people do not have providers near them who are skilled to attend them for a vaginal breech birth, it is ideal to try to encourage baby to turn head down.
Towards the end of pregnancy, the baby settles into its favorite position. Ideally, this position is vertex, meaning that its head is down towards your pelvis and its bottom is high up in your abdomen.
Less commonly, the baby is breech (with its head up and its bottom down towards your pelvis).
It’s not always known why a baby is breech at term. Sometimes it has to do with:
Relationship between the shape of the baby and the shape of mom’s uterus or pelvic bones
Location of the placenta
Issues with the umbilical cord
Excessive amniotic fluid
Lax abdominal or uterine muscle tone
Labor and birth does carry more risk of complications when the baby’s head is not down towards the pelvis, even though breech is a variation of normal. So, when a baby is breech by the 30th week of pregnancy they should be encouraged to convert to the ideal vertex position. That said, the majority do turn by themselves at the beginning of the ninth month.
What to do When Baby is Breech
If your baby is breech at 30 weeks, consider doing a couple of the following exercises 10-15 minutes 2-3 times each day until your baby turns.
Belly massage. Massage your abdomen GENTLY in the natural direction the baby will turn. But stop if you meet any resistance, and never attempt to forcefully turn the baby yourself.
Visualization. Close your eyes and imagine your baby with his or her head moving down in your pelvis.
Coaxing. Play classical or relaxing instrumental music by your pelvis, so that the baby will turn towards the soothing sound. Or shine a flashlight by your pelvis, so that the baby may move towards the light.
Go for a swim. Swim laps and do some handstands in the pool.
Pelvic rocking. Shift your pelvis up and down and side to side while on your hands and knees.
Act like an elephant. Walk around the house on your hands and feet.
Bridges and inversions. If you have an established yoga practice, go upside down with any of the inversions, using props for supportive modifications. Headstands and downward-facing dogs work wonders.
Beginners should start with bridges. To do this, simply lie on your back with your feet flat on the floor approximately 1 ½ - 2 feet apart and your knees bent. Elevate your hips 9-12 inches higher than your shoulders. You can support yourself in bridge with a yoga block under your sacrum.
Alternatively, lie on your front in the same “upside down” position, keeping your weight on your forearms and knees wide, with your bottom in the air. Lying on three pillows or a beanbag chair can help further elevate your hips.
Or, lie bent over the edge of a sofa or top of a staircase with your legs on the floor and your body lying down the sofa or stairs. Support your body with your hands or forearms so that your torso is inclined upside down.
Gently roll your hips side to side while in any of these positions.
Taking homeopathic Pulsatilla 30C will help the above exercises be more successful. Allow 4-5 pellets to dissolve under your tongue 3 times daily for 3-5 days. As with any homeopathic remedy, avoid eating or drinking for 15-20 minutes before and after.
Natural Remedies for Breech Babies
In addition to exercises that help your baby move into the best birth position, there are a few techniques that can be administered by care providers. If you’ve tried the above suggestions without success, look for a practitioner that practices one of the following.
MOXIBUSTION
Find an Acupuncturist or Doctor of Traditional Chinese Medicine who has had success turning breech babies to vertex with moxibustion. The technique involves burning certain herbs close to the skin at specific acupuncture points.
WEBSTER TECHNIQUE
A chiropractor trained in the Webster Technique can use this sacral adjustment to help facilitate the pelvic alignment needed for your baby to get into birth position.
MANUAL TURNING (External Cephalic Version)
If all else fails, you can opt for having your baby turned manually if the right conditions are met (such as no cord around the baby’s neck or short cord, adequate amniotic fluid, and healthy baby as detected on ultrasound with a normal fetal heart beat). Sometimes this is can be easily done in your birth practitioner’s office at 34 -36 weeks, especially in a woman who has delivered vaginally before, while carefully assessing the baby’s heartbeat. It has a high rate of success in skilled hands and supportive conditions.
Experienced midwives can turn breech babies. Most obstetricians prefer to do it in the hospital, often with medication to relax your uterus, ultrasound guidance, and continuous fetal heart monitoring. But it can safely be done out in of hospital settings while monitoring baby.
Ask for a wedge pillow to support you in a tilted pelvic lift position, or a bed that can be placed at an angle, with your legs higher than your head to help baby out of pelvis. Also, having it down while in deep meditation being supported in a pool of water has been effective and a wonderful experience.
Once the baby is turned to the head down position, stop inverting yourself, wear an abdominal binder at all times to prevent the baby from turning back to breech.
If your baby insists on being breech as you approach your due date, discuss your options with your provider. If they are not supportive of your choices for a vaginal breech birth, find a different practitioner, optimally one who has the essential skills and philosophy of birthing breech babies vaginally when appropriate and safe to do so. You can ask for recommendations at Breech Without Borders.
A baby lying in the transverse position, however, can only be delivered safely by cesarean section.
For more information on having the birth of your dreams, check out my Love Your Birth comprehensive signature prep course Guide to Pregnancy, Birth and Postpartum
If you desire personal guidance, schedule an online or in person coaching call with me.