My heartfelt thanks for reading my story. I'm so blessed and honored that you will post my birth story on your blog and social media. I hope and pray that this would inspire more women to try birthing naturally and perhaps encourage them also to sing and dance their way through labor!
I was diagnosed with Pre-Eclampsia with severe features due to the extremely high amount of protein in my urine. My blood pressure remained normal, below 120/80, all throughout my labor, delivery & recovery. This is my 5th pregnancy. My first pregnancy was with twins. The 1st twin, Annalise, was born naturally (no anesthesia, IV, oxygen, pain meds) in our church's birthing clinic. The 2nd twin, Therese, was born via CS in a hospital. I was transferred because Therese went transverse when Annalise came out and it was Therese's hand that first came out. My midwife put her hand back twice before transferring us to the hospital.
In most hospitals, 24 hour monitoring is only done in the High Risk unit, so when my fluid was low, I had to be monitored for a full 24 hours before I transferred to a regular room. I went back to the High Risk unit again for the Magnesium sulfate, to counter possible seizure or convulsions, according to my OB. They also don't allow the natural birthing suite for high-risk cases like mine, because I already underwent Caesarean in a previous pregnancy, even though I've already had 3 VBACs.
Valentine’s Day, Thursday, Feb. 14, 2019, I was looking forward to a lovely dinner that night with my husband of 13 years, Ritche, to celebrate our 15th year of being together, when we received news that my husband’s 98-year old maternal grandmother “Lola Auring,” whom he was very close to, had just passed away peacefully in her sleep. He regretted not being able to visit her sooner when she was still alive but looked forward to flying out from our home in Metro Manila (Philippines) to their province to be with her for the last time.
But, first things first… I had to go to St. Luke’s Medical Center in Bonifacio Global City, for my routine 36th week checkup & ultrasound. My OB did a Biophysical Score of our baby and told me that my fluid was low. In my mind, I thought, “Okay, I’ll just have to drink up at home then.” But, my OB had another plan... I needed to be admitted to the High Risk Pregnancy Unit and hydrate via IV. I called Ritche and he agreed for me to be confined, thinking we’ll just stay overnight until my fluid goes up in 24 hours.
So, aside from the IV drip, I tripled my water intake to 3 liters in the morning, 3 liters in the afternoon and 2 liters at night, which equated peeing almost every hour! AND I had to be hooked to several machines so my heart rate, blood pressure, baby’s heart rate and my contractions will be monitored for 24 hours. It was super uncomfortable but I thought, “No problem! As long as baby’s fluid will go up right away.” We then asked our churchmates and close family & friends to pray with us. I also prayed that I would be discharged as soon as possible so that Ritche could still travel the next day to be with Lola Auring.
24 hours later, Friday afternoon, my fluid just increased a tiny bit so my OB double checked the protein-creatinine ratio in my urine. While waiting for the results, we got a regular room and waited another 24 hours. My husband already cancelled his trip and let my mother-in-law, Mama Tess, go ahead to their home in the province. My UPC ratio was still extremely high, which made me a candidate for severe pre-eclampsia. We couldn’t believe it. Even my OB couldn’t believe it, either. I’ve always been careful with my diet, preferring veggies & fruits. I always made sure I had regular exercise. My blood pressure has always been normal. How could I have pre-eclampsia?
We’ve been praying for Baby Abe to come out at least on his 38th week so, imagine our surprise when she advised us on Saturday afternoon that we’ll both be safer if he came out as soon as I reach my 37th week, which was the following day, Sunday! Questions ran through my mind. We knew 38 weeks is the ideal. How do I induce labor? We’ve always just waited for me to labor naturally. With Agatha, our 5th child, we had to keep her in as long as possible. With Abe, it seems, we now had to bring him out as soon as possible! We hadn’t even packed our hospital bag! We were just supposed to buy baby boy stuff this week!
I had my Birth Plan printed out for the doctors and nurses and went back to the High Risk unit so that I can be given magnesium sulfate to counter possible seizure/convulsions. I was also given 4000 mg of Evening Primrose Oil every 4 hours to soften my cervix. It just seemed so foreign and unnatural to me that we had to naturally induce labor. How do we do that?
My husband comforted me and reminded me that we have a great and awesome God and that so many people are praying for us. He had been diligently communicating with and updating our close friends. My dearest friend Kartika from Singapore visited me twice. My best friend and sister, Lala and her husband, Solomon, came all the way from Carmona, Cavite, to encourage me with their love and presence. Our dear godparents, Fr. Dino and Sis. Anj, braved the 3-hour traffic to show their support and pray with us. When they mentioned the words “total trust” and “perfect peace” in their prayers, I was inspired by the Holy Spirit to write down the alliterations the Lord revealed to me as they were born in my heart so I can meditate on them:
“Total Trust in Thee” “Perfect Peace in the Prince of Peace” “Sweet Surrender to My Savior” “Calm and Courageous in Christ” “Blissfully Blessed and Brave to Birth our Baby Boy” “Relaxed, Rested and Ready”
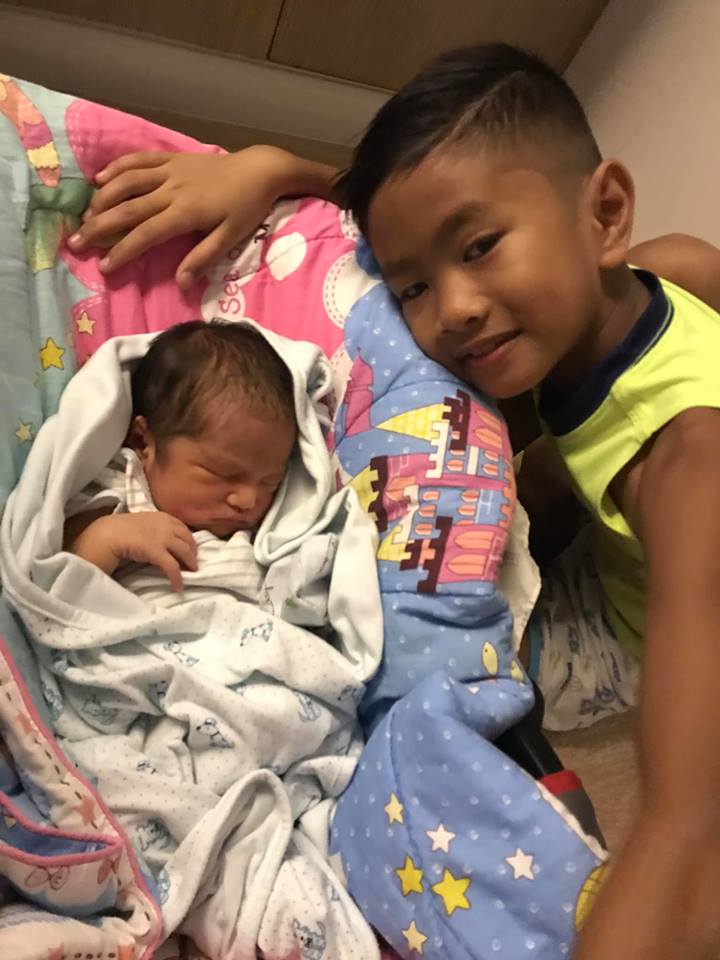
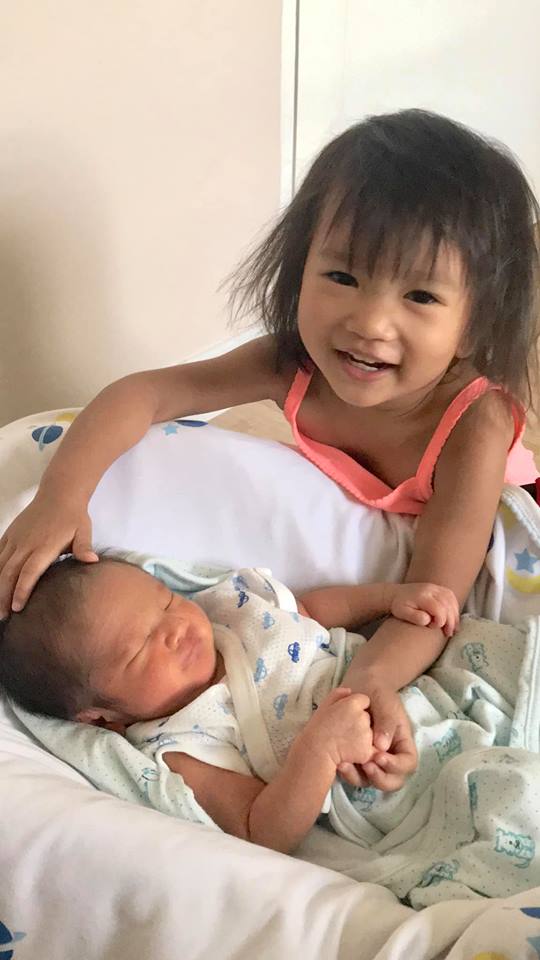
Most importantly, my mother, Mama Lou, my father-in-law, Papa Adelo, and our 5 beautiful and wonderful children, gave me so much encouragement that I knew that we can bring Baby Abe out in God’s perfect timing. The Holy Spirit will lead me and guide our baby out.
Monday, after the magnesium sulfate treatment, I had another ultrasound. Baby’s fluid had significantly increased from 7.89 to 13! Praise God! We could really feel the prayers of everyone. We were ready to induce natural labor. My OB mentioned that Baby Abe could even be born on Thursday, which was her birthday! But I thought to myself that I didn’t want to labor that long. Our churchmates, Dcn. Jojo and Sis. Evelyn, brought homebaked muffins along with much laughter and prayed over us before leaving.
We finally finished my IV (Yay!) and I drank my red raspberry leaf tea, walked about our windowless room, slow danced, bounced on a birthing ball. Contractions were very mild at 3-5 minutes apart, but they weren’t “painful.” Mama Chato, our midwife who helped me naturally birth our other children, taught us that we must reframe contractions as “good pain” because it helps bring the baby down. The more you welcome each “good pain” and embrace the sensation, the more relaxed you will be and fear will leave you. So, everytime I felt a contraction coming, I relaxed my facial muscles, my jaw, my shoulders and let the tightening sensation do its work on my belly. The uterus is a very powerful muscle and I looked forward to the pressure, imagining that every contraction brought Baby Abe closer to being in my arms.
The resident doctor did my first internal examination and said I’m only 2cm dilated. Well, at least it’s not totally closed, right? However, at 530pm, I had an unexplainable occurrence of “chills” where I suddenly felt like I was freezing. I couldn’t stop my teeth from chattering and my body from shaking violently. My mom wrapped me in thick blankets, wore socks on me, rubbed my legs. I called my husband to hurry, as he was getting some documents for our hospital stay. I placed my cold hands in my armpits and prayed that the nurse won’t peek in and report that I’m having some kind of seizure. The chills passed after 20 minutes. My husband warmed me with his embrace. However, I couldn’t sleep a wink that night. My husband decided we transfer again to a normal room with windows so I could be more comfortable. I searched online “how to dilate cervix fast” and visualized my cervix opening and prayed constantly to the Lord to give me thoughts of peace and not anxiety. The baby knows when to be born.
Tuesday, I had a prenatal massage to relax and press those labor-inducing points, drank more red raspberry leaf tea, bounced on the ball and did more than walking, I did some dancing, too! Contractions were still mild at 3-5 minutes apart. I had another bout of “chills” at 530pm so my mother wrapped me again and I rebuked every thought of convulsion or seizure. I kept telling myself that this will pass and Baby Abe is safe in my womb. The chills stopped at 6pm. By 8pm, I was so tired from the lack of sleep that I was able to sleep very well, even with the regular rhythm of my belly tightening. We continued to entrust everything into the Father’s hands.
The next day, Wednesday, February 20, I was determined to up my natural induction techniques. My OB was pleased with the progress of my labor but reminded me not to wait until my water broke. She reminded me to let her residents know when I’m already 4cm dilated, because I gave birth so quickly to our last child, she almost didn’t make it.
My Mama Lou and I danced belly, hip hop, Zumba to the jiggiest songs I could find (Think “Trolls” soundtrack, “Walking on Sunshine” “Moves Like Jagger” “Waka Waka” you get the picture) and I sang my heart out to our Hillsong & Bethel favorites (Oceans, What a Beautiful Name, O Praise the Name, Open Heaven/River Wild, It Is Well, No Longer Slaves, etc.) when I rested. The doctors and nurses were amazed I could still sing and dance through my contractions. Haha! It actually took my mind away from the pressure. By 530pm, I thought my water was leaking so I called a resident to examine me. No water, just the EvePrim Oil melting but I was 3-4cm dilated. Yay! She then asked me to go down to continue laboring in the High Risk unit. Labor progressed very quickly and I did feel more and more pressure every minute!
Shout out to the doctors and nurses of St. Luke’s BGC for honoring my Birth Plan as much as possible and I agreed that I will only be hooked to the monitor for 20-30 mins every 2 hours.. No pitocin, no IV, no oxygen and no pain meds. By 8pm, I was 5cm dilated. Hooray! That pushed me to do even more dancing, bouncing, marching, swaying & singing during contractions, with my husband playing every song I requested. The pressure was already immense at this time, and I had a tugging feeling I was very close to transition, although it’s only been a couple of hours. I was thankful that my husband was just right there to tell me I’m doing great, and my mother was also with us, cheering me on. Whenever I felt the tremendous pressure, I would say, “Baby’s going down, down, down! Yes, yes, yes! Go, go, go!” and I knew that they both agreed with me and believed with me.
I was already speaking in tongues, asking the Holy Spirit to be my Comforter, my Teacher, my Guide. I envisioned Mama Mary giving birth to our Lord and Savior Jesus Christ. I remembered all our children who are happily awaiting their baby brother at home. They’re counting on me to give birth to Baby Abe soon. I wanted to birth this beautiful being in my womb without fear, only love and joy and peace... Feelings of indescribable bliss welled up in my heart for this boy whom Ritche and I had so conceived in love. I was determined to confidently bring him out in that same love that conceived him.
At 1030pm, I asked the resident to check my cervix, which had already dilated to 7cm, with a “bursting” effacement. I had to be strapped again so I lay down waiting for the nurse when, a minute after, the nurse relays the message from the doctor to tell them right away if my water bag ruptures. She hadn’t left the room yet when my water bag burst! It felt like a water balloon popped out of me.
I excitedly told everyone, “Baby’s coming out!”
They wheeled me out our room into the delivery room right away. I felt the head of Baby Abe crowning.. I thought I couldn’t hold him in anymore.. but I tried to relax, as the doctors were still preparing, I had to be moved from my bed to the delivery bed and my husband, Ritche, was also getting into scrubs. I requested that I be more upright and not lying down. Our OB was nowhere to be found but already gave instructions to her three resident OBs present in the room. I already felt like pushing but was holding Baby Abe in.. I was so excited.. I called my husband.. “Daddy!” and told the nurse, “The cellphone!” Haha! I didn’t want the nurse to miss taking Daddy Ritche’s picture catching Baby Abe.
Finally, it was only a matter of minutes before I told them I had to push Baby’s head out. The doctors assured me and said they won’t hinder me from pushing. His head came out and the doctor was wise enough to remind me not to push anymore because he slid out so easily! It’s a birth phenomenon they call the “Fetal Ejection Reflex.” Pushing would have made the baby fly out.. Haha! It was amazing to see my husband “catching” our son! As with all our other children (except Therese who underwent emergency CS), he did the ceremonial cord cutting after the cord stopped pulsating. Baby Abe had already pooped meconium but miraculously, he didn’t ingest any and his Apgar score was 9 out of 10. Thank God!
I delivered the placenta within 5 minutes. And our OB, Dra. Bambalan, arrived moments after to check on me. Everything looked good. My blood pressure stayed normal all throughout. I had a 1 mm tear that didn’t need any stitching.
They were amazed at how easy the birth was and how fresh I still looked even after giving birth. We all laughed at how my primary concern was to get the cellphone to the nurse and how Baby Abe didn’t want to have the same birthday as Doc. Everyone in the room was lighthearted and Dr. De Guzman exclaimed that this was one delivery she will never ever forget!
All in all, we stayed in the delivery room for 18 minutes then I was brought out to the Recovery Room for 4 hours to check on Baby Abe and me. By the end of the recovery period, my BP was still stable, Baby Abe and I had skin to skin contact and he latched on the breast perfectly, but there was just one problem. The nurse said that they’d have to put a catheter on me if I didn’t urinate soon. No way! I gently pressed on my bladder and, sure enough, I was able to pee on my own.
The next 48 hours were critical for me and Baby Abe. I recently saw the diagnosis of my OB upon discharge. It was Pre-eclampsia with Severe Features. But, thank God, we never manifested any complications. No headache, nausea, vomiting, seizure, swelling, convulsion, shortness of breath whatsoever. My blood pressure never elevated all throughout. Baby’s oxygen levels were stable. I didn’t go into shock, stroke, had brain damage or any organ failure. I didn’t need any kind of pain medication.
Within 48 hours of delivery, we went home to our family, carrying our 6thbundle of joy, our second boy, whom we named "Abraham Nickola." So thankful to all our family, relatives, friends, and churchmates for keeping us in your thoughts and lifting us up in prayer. I believe that Ritche’s grandmother, Lola Auring, was also looking down from Heaven and interceding for us, along with all the saints and angels. To God be all the glory, honor and praise! He is a miracle-working God who faithfully keeps all His promises and grants us the desires of our hearts!
By: Chat Jandayan @chatjandayan
Most of the photos were taken by my husband and my mom.
This is why excellent childbirth education is a must, why planning for your birth and the unexpected challenges that can arise, is so important today, and is a major reason why I created my Love Your Birth course. It is a comprehensive online course that teaches women what they need to know about planning and carrying out the birth that they want in all settings - the hospital, birthing center or at home. It’s a course on how to have a holistic, healthy pregnancy for the body, mind, and soul - and is how I have guided thousands of women and their families in my midwifery practice for over 21 years.
It contains a rolodex of my favorite resources with over 200 of the best books, movies and supplies I use personally and professionally with my clients, family & friends. Even diving into a fraction of this list will have you feeling empowered and prepared for conception, pregnancy, postpartum and parenting...It includes resources on improving and even ensuring ensuring healthier pregnancy and birth outcomes than the status quo, and preventing and healing from birth trauma so prevalent in the modern world!
Be prepared to do some research on your own, but knowledge restores your power. I also help you prepare your mindset for such a task, to debunk myths, and to reframe any current ideas or conditioning about pregnancy and birth that can use a change in perspective or that are simply incorrect and do serve you. After finishing the course, the idea is that you are now able to create and have the healthy, beautiful and empowering pregnancy and birth that you want - so you can ROCK your birth, however it unfolds!
It’s wonderful alone, a great refresher or adjunct to any other course!