How to Deal With Fatigue During Pregnancy
Fatigue during pregnancy is a very common experience. Growing a baby is an enormous task and requires a tremendous amount of physical and mental energy.
There are a number of factors that can contribute to fatigue during pregnancy:
The increased demands on your body, mind and spirit.
Lack of quality sleep or rest periods.
Overworking yourself inside and/or outside of the house.
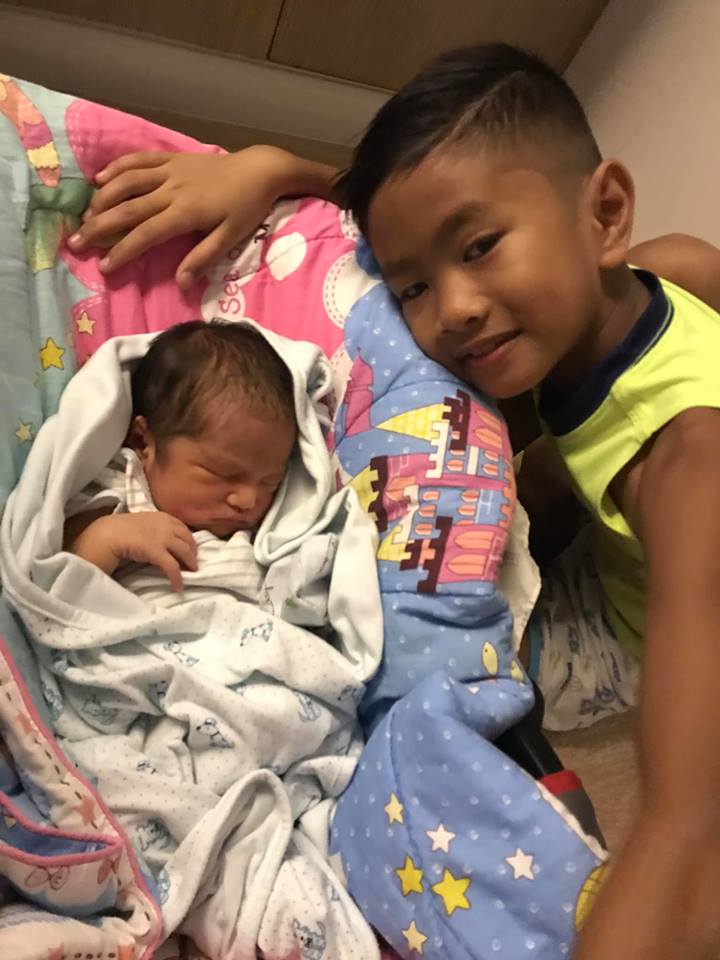
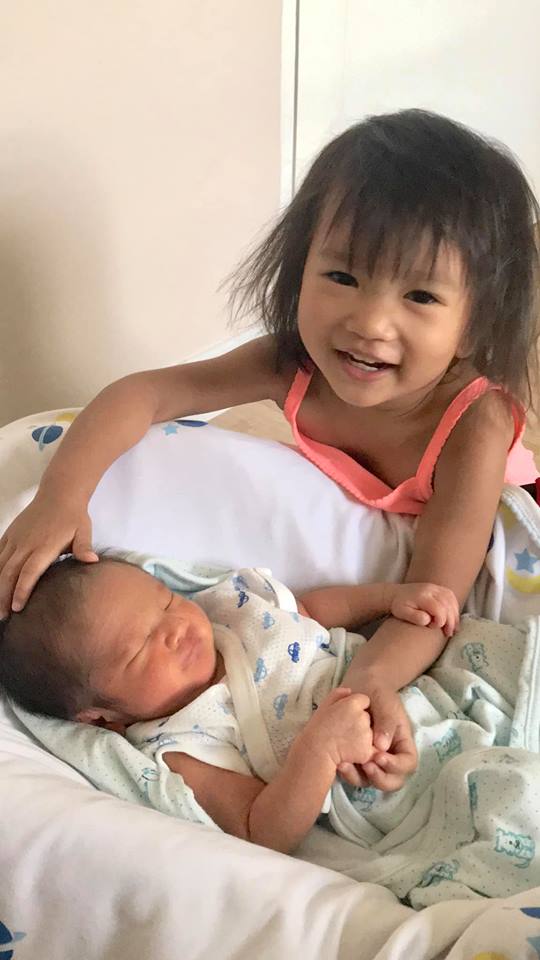
Short pregnancy spacing, breastfeeding and caring for other children
Too much time on computer or cell phone.
Inadequate diet.
Sedentary living.
Unexpressed or unresolved emotional difficulties.
Depression or anxiety.
Anemia.
Acute infection or illness.
Under-active thyroid function.
Other health problems.
And even boredom.
Resolving Fatigue During Pregnancy
Look at the whole picture. Consider what in your life could be contributing to your fatigue, and take common sense measures to take care of yourself.
LACK OF REST
Get more sleep by going to bed earlier, sleeping later in the morning and/or taking a nap during the daytime. Getting enough sleep is especially essential during pregnancy.
Take frequent breaks or “healing intervals” throughout the day to simply sit down, rest, center and calm yourself. You can do this by sitting quietly with your eyes closed, slowing down your thoughts by focusing on slow deep breathing while gazing internally between your eyebrows.
Meditation, breathwork, visualization, and yoga nidra/progressive muscle relaxation are all great ways to relax the body. There are many books, audio CDs and hypnobirthing MP3s for pregnancy to help you learn these important life skills, and now there are wonderful phone apps like Breathe and Calm. Make it a regular part of your daily routine to practice them - even just for 15 - 20 minutes.
INADEQUATE DIET
Paying close attention to your diet can go a long way in avoiding fatigue during pregnancy, as your nutritional needs soar during this time.
Make sure you’re drinking 8-10 glasses of filtered, spring or well water daily. Try to drink water away from meals (at least 20-30 minutes before or 2 hours after). Include in your daily diet plenty of fresh organic fruits, vegetables, whole grains., lots of protein and healthy fats.
Eat 20-30 grams of protein three times daily such as:
Beans
Nuts and nut butters
Seeds
Tempeh
Organic whole eggs
Wild Alaskan Salmon
Turkey or chicken
Beef, Lamb and Buffalo
Organic fresh raw whole dairy - ideally goat or sheep
When eating fruit and whole grains, combine it with a protein or fat like avocado, nuts or nut butters, eggs, or a piece of organic cheese. If eating whole-grain carbohydrates makes you tired, reserve them for your evening meal.
Use cold expeller pressed extra virgin olive and/or coconut oil, and butter (goat is best) as your primary fat for cooking.
Eat small amounts several times throughout the day rather than heavy infrequent meals.
Products containing refined white flours and sugars or high fructose corn syrup will give you a temporary energy boost, followed by greater fatigue once the effect wears off. These should be avoided.
Also avoid highly refined processed foods, as these are usually void of nourishment and contain all sorts of chemicals, unhealthy fats, simple starches and sugars that can also make you feel more tired after an initial brief boost in energy.
VITAMIN AND MINERAL DEFICIENCIES
If you are anemic (which is very common in pregnancy, especially during the second and third trimesters), eat iron-rich foods. Good options include eggs, dark green leafy vegetables, seeds, nuts, beans and split peas, dried fruit, iron fortified cereals, red meat and poultry, blackstrap molasses, and brewers yeast. Take natural herbal sources of iron, such as Floravital Iron & Herbs - it comes in liquid and tablet form, as needed. There are other wonderful natural remedies to boost iron in my online holistic apothecary. Most of the supplements and herbal remedies I recommend are available on my customized online holistic apothecary. Find the best supplements that have gone through my thorough screening process there. Look in the category for fatigue or search them individually. My online dispensary is a convenient way for you to purchase my hand-picked, professional-grade, whole food supplements and other natural health products. Ordering is simple, and the products will be shipped directly to your home or work within a few days.
If your vitamin B 12 levels are low (common in women who have had several successive pregnancies or are breastfeeding), supplementing with 1000 mcg will be needed and can really make a huge difference in how you feel. It is also in the apothecary.
Also, be sure to take a good all natural whole-food based prenatal vitamin and mineral supplement.
A daily nutrition-rich fresh juice made with a combination of veggies and superfoods like spirulina, kelp or wheatgrass can help you feel more alert and energized. Start slowly with 1-2 tablespoons of the superfoods and build up to 1-2 ounces. Drink first thing in the morning on an empty stomach. Superfoods also come in all natural powdered mixes that can be added to your daily smoothie. Note: if you have a lot of accumulated toxins in your body, wheatgrass may cause slight nausea at first as it cleanses your system. This is harmless and eventually passes.
NATURE AND MOVEMENT
Get plenty of fresh air and adequate exposure to sunlight on a daily basis. Try to spend at least 20 minutes outside with nature in the early morning or late afternoon sun each day without sunscreen. If spending a lot of time indoors, at least open the windows – even and especially in the winter.
Engage in moderate exercise for 30 minutes at least 5 days per week. Good options during pregnancy include swimming, brisk walking, cycling, dancing, or low-impact aerobics. Even though you feel tired, exercise creates energy and does wonders to minimize fatigue, depression and anxiety. Incorporating yoga (especially prenatal, Yin, gentle, and restorative) as a regular part of your daily routine can also be very powerful.
Try to maintain correct posture and body mechanics. Use your abdominal muscles to straighten your upper back and tuck your pelvis in to straighten your lower back. Engage your core by bringing your breast bone and lower ribs and belly toward your back, and bringing your front pelvic bone towards your breast bone. Use your arm and leg muscles instead of your weaker back muscles to lift, carry, pull, and push things.
EMOTIONAL HEALTH
It is important to be open and honest about your feelings to yourself. Some women find it helpful to keep a journal or diary to increase self-awareness and understanding. Share your feelings with your spouse, close friend or family member. Periodically release pent up emotions with a good cry, followed by a hug.
Move strong emotions through your body. If you are angry or overstressed, play an angry song, if you feel grief, play a sad song, or simply play a track of African drumming and let your body move to the music, while making the sounds you need. Our little ones have their temper tantrums, move and release their emotions so they are not repressed and stuck in their bodies. Then they get up and play. Indigenous cultures dance their grief, anger, joy and celebration in community drum circles. We have much to learn from them. Invite friends and have your own drum circle to express and release emotions - you might just feel so exhilarated by it you will want to do this regularly.
Avoid overexertion and trying to be “super mom” by re-examining your priorities, limiting unessential activities, and learning how to say “no.” Delegate tasks to others and let friends and family help.
Try to allow yourself regular time each day without guilt to do something that you fully enjoy, that inspires and uplifts you. Make it easy and fun. Some ideas are:
Watching a musical, romance, comedy or inspirational drama
Reading a good novel
Taking a stroll through the park or in a beautiful spot in nature
Gardening
Going on an outing with your partner or good friend
Cultivating a hobby you desire
Learning something new that interests you
Add more laughter and play to your life. Many women are surprised to find how health-enhancing and energizing this can be.
Seek out a transformational life coach or, if needed, a professional holistic therapist if the above ideas do not help and you are troubled by psychological distress or emotional discomfort. Suppressed feelings can worsen fatigue as well as cause all sorts of other problems if not properly dealt with.
HERBS AND OILS
Take an invigorating bath with a few drops of essential oils of peppermint or eucalyptus, lemon, wild orange, grapefruit and/or rosemary. You can add a few drops of these essential oils to a bowl or spray bottle of cool water and splash or spray yourself with the uplifting scents throughout the day.
Nettle is a great herb to be taking in pregnancy as a nourishing tonic. It also has the added benefits of blood sugar regulation, adrenal support, improving nutrient intake, and building iron levels. Make a strong infusion by steeping a handful of dried herb in 1 quart of boiling water for 3-4 hours and strain into a canning jar. Drink 1-3 cups daily (with fresh lemon or lime juice, mint leaf or a dash of honey to taste). A fresh spearmint or peppermint tea can also provide a lift of spirit and energy.
If interested in other herbs to improve energy, combine equal amounts of herbal tinctures of schisandra, eleuthero, and American ginseng, and take 1/4 to 1/2 tsp once or twice per day. Start with the lowest dose and work your way up as needed. Reputable herbal companies include Gaia, Eclectic Institute and Wish Garden.
Minimize or avoid caffeinated coffee. It is addictive, too much is harmful, the energy boost is artificial, and it can be agitating and impair sleep. Many feel more tired when its effects wear off.
Avoid stimulant drugs (including diet pills) and sleeping medications, as most have side effects for you and your growing fetus, and can cause you to become dependent on them. Many substances, such as cocaine, are outright dangerous to you and your baby. You must seek professional help if you cannot stop using them.
OTHER RESOURCES
Homeopathy and acupuncture can both be great for soothing stress and increasing energy. Also, check out Clarity Breathwork and/or read The Journey. - for extremely effective, mind-body, cutting edge methods that have lead to transformational healing for thousands of people around the world.
If you experience any sort of chronic fatigue and exhaustion in which serious causes have been ruled out and none of the natural and allopathic remedies help, consider reading the book “The Mindbody Prescription” by Dr John Sarno, MD, an amazing pioneering physician whose brilliant approach has helped hundreds of thousands of people without drugs, physical measure or surgery.
If your exhaustion is extreme or persists in spite of following the above guidelines, consult your physician or midwife or schedule a consultation with me. If you are feeling overwhelmed, or do not even know what questions to ask, I can help you!
Check out my number one international best selling book Natural Birth Secrets and my online course - an online version of how I have helped thousands in my local practice. Both resources are unique, but each provide an in depth, one-of-a-kind holistic approach created by me, a seasoned nurse midwife of over two decades, who has seen everything!
Battling with low back or pelvic discomfort? Having common pregnancy aches and pains and need some additional support? Try Bellefit’s prenatal support wear. You can check them out and purchase here.