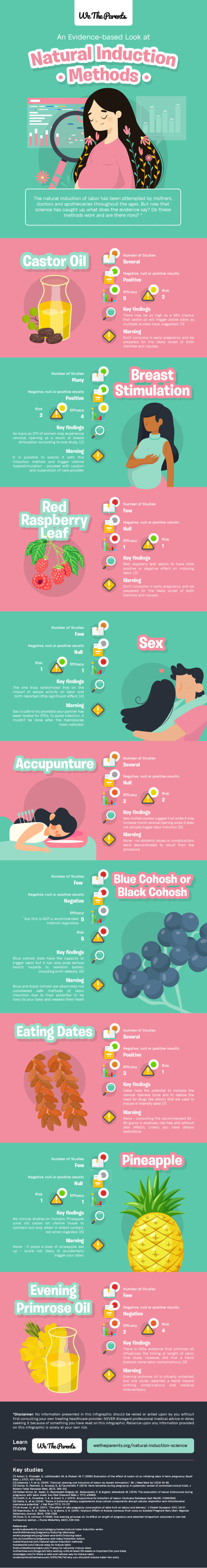
Art by Katie Atkinson @spiritysol
A baby in a posterior position is facing your abdomen, and baby’s back is towards your back. Some babies are born easily in the posterior position with baby facing mama’s face “sunny side up.” This is especially if Mama:
Has given birth before
Is carrying a baby of average or smaller size
Has an adequate sized pelvis
Is committed, relaxed and prepared
Is able to be upright, move and change positions at will
Has the ability to eat and drink freely
Is supported by providers who are patient, calm and trained to help baby turn
Art by Katie Atkinson @spiritysol
Other babies in posterior position can be more challenging, creating problems like not going into labor, water breaking prematurely before labor starts, slower more difficult labor progress, exhaustion, and labor felt mostly as back pain that can be harder to cope with. All of these factors increase the risk of complications, interventions and cesarean if baby can not be safely born vaginally.
Epidurals increase the incidence of posterior babies, as well. But sometimes in prolonged labor, when Mama can no longer cope, the compassionate use of an epidural can help her give birth vaginally.
The modern sedentary lifestyle of slouching in chairs over smart phones and computers, sitting back in sofas and car seats with associated poor posture, stress and tension in our bodies contributes to the rise in babies presenting in the posterior position. Many of us are no longer as active as our ancestors and indigenous cultures around the globe. We are not often leaning forward doing manual work, which helps baby’s heavier back come forward into the anterior position, unless we are doing activities like gardening.
Art by Katie Atkinson @spiritysol
Ideally and actually most often, the baby will be in an anterior position facing your spine at term, or turns anterior during labor for childbirth. It is important to know when your baby moves into the optimal anterior position, so you can encourage the baby to stay there, which usually means an easier and shorter labor.
You can learn on your own what position your baby is in. But if you are unsure, ask your practitioner for help figuring it out. Then try to pay attention to your baby’s position, without getting needlessly obsessed about it. This is easier to do when your baby moves or when momentarily lying on your back. It may take a lot of concentration to understand what is what at first, but soon you will get the hang of it.
When your baby is posterior, your tummy may look flatter and feel more squashy, and you may feel arms and legs and kicks all over the front towards the middle of your tummy. The area around your belly button may dip to a concave, saucer-like shape, and you may also experience long and painful practice contractions with a more severe lower backache as your baby tries to turn around to the anterior position to engage down into the pelvis.
When your baby is anterior, the back feels hard and smooth and rounded on one side of your tummy, and you will usually feel kicks under the side of your ribs. Your belly button will normally poke out and feel firm.
Pay attention to your posture and positioning at the time when your baby may be starting to descend into your pelvis, which is during the last 6 weeks of your first pregnancy, and the last 2-3 weeks of your subsequent pregnancies. The goal is to make room for your baby to assume the optimal position for birthing.
The baby’s back is the heaviest side of its body, and will thus gravitate towards the lowest side of your abdomen. So, if your tummy is lower than your back (such as sitting on a chair leaning forward), the baby’s back will tend to swing anterior towards your tummy.
If your back is lower than your tummy (such as reclining back in an armchair with your feet up), then the baby’s back may swing towards your back into a posterior position. With this in mind, when you are 34 weeks onward, avoid any position where you are spending time leaning backwards with your knees higher than your pelvis.
Ideally, ditch the chairs. If you do need to sit on one, make sure your knees are lower than your pelvis, and your trunk is tilted slightly forward. If you need to work at a desk, consider a standing one at least some of the time, resting an alternating foot on a step stool.
Watch TV, read and lounge while kneeling on the floor, over a beanbag, birth ball, cushions, or sitting backwards on a straight backed dining room or kitchen chair facing and leaning on its back.
Practice yoga to be in shape for the lunges and varied positions used to help your baby come down and out. Use yoga positions like bound angle (badha konasana) sitting with your back upright with soles of your feet together, or on your hands and knees while curving your back up like a cat followed by dropping your spine down in an arch and/or wiggling your hips from side to side. Get out your yoga mat and support your body with props like blankets, bolsters or blocks as needed.
Avoid crossing your legs, as it reduces the space in front of your pelvis and opens up the back. Sit on a wedge cushion in the car so your pelvis is tilted forward, and keep the seat back upright.
Avoid deep squatting until baby is anterior and well down in your pelvis or when needed in labor. Deep squatting opens up your pelvis and encourages the baby to move down, so refrain from it until your baby is in the anterior position. You can squat on a low stool or yoga blocks instead, keeping your spine upright.
Rest and sleep on your side, with two pillows under your bent right knee, which should be jackknifed up towards your chest, and keep your left leg straight out.
Swim with your belly downwards, doing the front crawl and breaststroke. The leg movements with the breaststroke in particular are great for opening your pelvis and encouraging your baby into an optimal anterior position.
If Your Baby Is Posterior
Continue the above mentioned positions, and add the following exercises for 20 to 30 minutes each, 3 times daily while watching something inspirational, romantic or that makes you laugh, or while listening to music:
Maintain a knee-chest position, with your buttocks sticking up in the air to tip the baby back out of the pelvis so there is more room to turn around to the anterior position.
Sway your hips back and forth and do the pelvic rock up and down while on your hands and knees.
Crawl around the floor on your hands and knees, or hands and feet like an elephant.
Scrub your floors or do some gardening.
Swim belly down, kicking with straight legs only. Avoid frog leg movements.
Lie on a slant board (using an ironing board or see-saw), with your head down and your legs up or lay with your pelvis and legs on the top stair landing or sofa and rest on your hands or forearms on a lower stair so you are at a similar incline. Jiggle your pelvis as you do this.
Try resting and sleeping on your tummy using lots of pillows and cushions for support.
Sit on a kneeler-rocker, which is a kneeling stool that sits you in an upright position with your knees lower than your chest, and has a rocker underneath for movement that encourages your baby to rotate. There are several types. See what is best for you.
When baby turns to the anterior position, you can encourage descent further into your pelvis by walking around upright, gently massaging the baby’s buttocks downward, deep squatting and swimming, this time using lots of breaststroke frog leg kicking.
If you have lax abdominal muscles from several babies or lack of toning exercises, use a supportive maternity binder to keep baby in place. Bellefit makes a fine one, as pictured below. You can check them out and purchase here.
If Going Into Labor With a Posterior Baby
Starting in early labor, try the following movements involving altering the level of your hips, which help wiggle the baby down through your pelvis:
Walk up and down stairs, sideways if you need to.
Rock and dance from side to side.
March or tread in place.
Step on and off a step stool.
Climb in and out of the birth pool.
Lay on your side, so the part of your belly where your baby’s back is, can lean forward almost over the sofa or bed, with your upper knee resting on a lower chair.
Consider having your midwives help to rotate the baby using a variety of external techniques, or if needed, by manually lifting your baby out of your pelvis during a contraction.
During the pushing stage of labor:
Kneel on all fours, with the other leg up in a lunge. Switch legs periodically. You can do this standing, alternating one leg up on a chair moving towards and away from it.
Maintain a supported high squat in a birthing stool or hanging from a dangling squatting rope or your partner, with your bottom at least 18 inches off the floor.
You can rest on your side with one leg straight out and the other leg bent up towards your chest, supported with pillows.
Avoid lying back, semi-reclining, sitting or semi-sitting.
For more information online, visit Spinning Babies, Association of Radical Midwives, or the GentlleBirth archives for Suboptimal Fetal Positions.
Check out my number one international best selling book Natural Birth Secrets and my Love Your Birth course, an online version of how I have helped thousands in my local practice.
Both resources are unique, but each provide an in depth, one-of-a-kind holistic approach created by me, a seasoned nurse midwife of over two decades, who has seen everything! It is now recommended by midwives, physicians, health care professionals around the globe, and doulas take it for their certification training.
As always, if you need more personalized guidance, schedule a consultation with me.